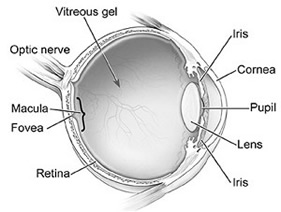
Before undergoing Vitreoretinal Surgery, it’s important to understand how the eye works.
Courtesy of National Eye Institute
How the Eye Works
Light rays enter the front of the eye through the cornea and lens. The cornea and lens bend the light so that it can be focused on the retina at the back of the eye. The retina is where the image is formed.
The iris, the colored part of the eye, changes the pupil size based on the amount of available light.
The pupil is the dark hole in the center of the iris.
The middle of the eye is filled with a jelly like substance called the vitreous. The vitreous is clear and allows light to pass directly from the front to the back of the eye.
The retina is at the back of the eye and is a light sensitive layer which consists of rod and cone cells. These cells collect the light signals and send them as electrical signals to the optic nerve at the back of the eye.
Rod cells are around the edge of the retina. Cone cells are concentrated in the center of the retina and where the light is focused by the cornea and lens. This is called the MACULA. Cone cells give us the detailed vision and most of our color vision.
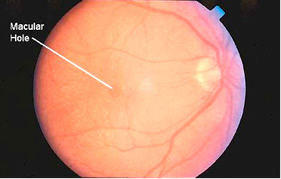
Macular Hole
Courtesy of North Shore Eye Centre (www.northshoreeye.com.au)
A macular hole is a small hole in the macula, located in the center of the eye’s retina. The macula provides the sharp, detailed vision we use for most things such as reading, sewing and driving. Other names for a macular hole are a macular cyst, retinal tear and retinal perforation.
Macular holes are normally caused as part of the aging process. As a person ages the vitreous, the clear gel like substance in the middle of the eye, becomes thicker and stringier. The vitreous contains millions of fine fibers that are attached to the surface of the retina. As the vitreous becomes thicker it begins to shrink and pull away from the retinal surface. Normally fluid fills this area where the vitreous has contracted.
However, in some people, as the vitreous pulls away it can tear the retina and create a macular hole. The fluid that has replaced the shrunken vitreous can seep through the hole onto the macula causing blurring and distorted vision.
Macular holes can also be caused by eye disorders such as high myopia (nearsightedness), diabetic eye disease, macular pucker, retinal detachment, Best’s disease or eye injury.
Symptoms
The symptoms of a macular hole include a slight distortion or blurriness in straight ahead vision in the early stages to a small blank patch in the center of vision in later stages. Reading or other routine tasks may become difficult.
Stages
There are three stages to a macular hole:
Stage 1 – Foveal detachment – In this early stage it is possible for
the macular hole to heal itself. About 50% of stage 1 macular holes
will progress further.
Stage 2 – Partial thickness holes – Most stage 2 macular holes will
progress further without treatment (about 70%).
Stage 3 – Full thickness holes – At this stage most central and
detailed vision is lost. Left untreated a stage 3 macular hole can
lead to retinal detachment.
How a Macular Hole is Treated
A surgical procedure called a VITRECTOMY is used to treat macular holes. In this surgery the vitreous gel is removed from the eye to prevent it from further pulling on the retina and is replaced by a gas bubble. Because the bubble is lighter than air it acts as an internal, temporary bandage that presses the macular hole flat onto the back of the eye.
Following the surgery, in order for the bubble to keep the macular hole closed, the patient must remain in a face down position for several days to several weeks. This position allows the bubble to press against the macula and to be gradually absorbed by the eye, sealing the hole. As the bubble dissipates the vitreous cavity is refilled with natural eye fluids.
The face down posturing is extremely important and is critical to the success of the surgery. It is important that you discuss any issues with your doctor regarding face down posturing prior to the surgery.
Certain precautions should be observed when there is a gas bubble in your eye. First of all you must remain face down as much as possible. Do not look straight up or lie on your back for any significant amount of time to minimize the anterior movement of the bubble, which can accelerate cataract formation, raise intraocular pressure or damage the cornea. Also avoid flying or climbing to a much higher altitude (ie. up a mountain). The reduced atmospheric pressure causes the bubble to expand which can raise the pressure inside the eye to a dangerous level.
If you cannot remain face down for the required length of time you may not be a good candidate for the surgery. McFee Technologies offers the most complete line of equipment to help you remain face down comfortably.
With close adherence to the face down posturing success rates for the surgery approach 90%.
Preparation for Face Down Positioning
Successful face down positioning after the surgery starts by being prepared. Plan on starting the face down positioning immediately after surgery, including on the trip home.
The following tips will help you have a successful outcome:
- Order and receive your post operative face down equipment in advance, have it arrive and set up prior to leaving for surgery. Make sure you are comfortable with the equipment and have had any questions answered by the supplier of the equipment.
- Take any necessary equipment with you such as the equipment for sleeping (if you have an overnight stay in the hospital or a nearby hotel) and any equipment for traveling (such as the McFee Medical Technologies travel cushion).
- Do any household chores such as cleaning, paying bills and shopping.
- Prepare meals in advance that can be micro-waved for easy heating.
- Make sure the house is clear of clutter so you can get around without falling.
- Pick up a supply of movies or audio books.
- Have a supply of tissues and anything else you may need close to where you are going to use your face down equipment.
- Have a supply of drinks close by to refill your water bottle that you received from McFee Technologies free with your order.
Tips for a Successful Recovery
Vitrectomy surgery is a easy, painless procedure with a successful track record of improving or virtually restoring vision. The real challenge for the patient is dealing with the monotony, stress, and discomfort of maintaining the face-down position on a continuous basis for several weeks.
Before the Operation
Before your vitrectomy, make sure to understand the procedure being done to you. It is crucial to prepare for the vitrectomy and the recovery so you will not be staggered later on. Sharing your complete medical history with your doctor is very, very important. Little things like seasonal allergies may potentially increase the amount of swelling from the accumulation of fluid in the sinuses. Ask your doctor questions. If you don’t understand the answer given the surgeon has given you, ask the question again. It is helpful to have a list of written questions and space for the answers ready prior to each visit. Try not to feel overwhelmed; when it comes down to the facts, this is a simple procedure.
It is much easier to get your home set up before the surgery. Prior to your surgery, you should take care of your chores such as paying bills, and doing enough laundry to supply your clothing needs. You may choose to prepare meals that are easily frozen then thawed such as casseroles. Remember, your face down positioning starts when you leave the operating room. It is helpful to proactive your positioning for a few hours at home prior to surgery to get adjusted to any problems in advance.
Once you know what will be done during the vitrectomy, it is wise to prepare and know about the healing process after the surgery.
What to Expect Post-Operatively
There might be swelling and tenderness (sometimes bruising) around the outside of the eye. You may feel pressure at first, but expect pain. Uncontrolled pain may hinder the immune system that aids healing and fights infection, so keeping your pain under control may be necessary to help you heal faster. “Leaking” from the tear duct is initially uncontrollable and normal, so if you experience this side effect, placing some tissues near your bed and chair is advised. Sleeping pattern tends to change with many patients. We suggest for you to take periodic naps so you do not become over-fatigued. Some may experience changes in taste, smell, and noise tolerance. Lack of depth perception may be difficult; you might discover the safety issues involved. Try to structure your living space as open and safe as possible.
Daytime Activities
Compliance is everything, especially in vitrectomies. It is also one of the most difficult to achieve. Keep yourself distracted and the things you use the most (tissue, snacks, drinks, etc.) should be closest to you physically. Taping lunch-sized bags to the chair and armrest for used tissues will eliminate the need for multiple, space-grabbing receptacles. Ask for and accept help from friends. Expect good days and not so good days. Don’t expect too much of yourself and try to be positive; it helps the immune system. Identify what comforts you and do it often. Above all communicate with your doctor; there are usually solutions to problems you haven’t thought of or don’t know.
Eating and Drinking
You should avoid bringing your chin to your chest as you eat, since this may affect swallowing. It is easier to bend at the waist and less with your neck for comfort while eating. A low TV tray, stool or coffee table will serve as excellent platforms. Prepare softer foods that are easier to chew and swallow with your head down. Keep refrigerated items on the lower shelved, and food on the counters, not up in cupboards. Do not raise your head to drink. Instead, use a straw. The low table that you use to eat from may also be in ideal place to rest your glass. (If you take oral medications that are difficult to swallow, you may need to break them into pieces, or mix them in soft food. They can also be dissolved in apple juice or other liquids.)
Bathing and Clothing
It may be easier to take a bath rather than a shower with your head down. A hand held shower massager can be very useful. Rearrange your soap, shampoo, etc. to a lower level so that you can reach them easily while bathing. During your period of face down positioning, wear a button-up shirt and avoiding sweatshirts, T-shirts and anything that will be required to pull over your head. Things that you can easily slip on and off, such as sweatpants, shorts, bath-robes, house coats and pajamas are recommended and will make your day easier.
Bathroom
You may need to use a laxative if you are prone to constipation, due to the relative inactivity during this period.
Night-time Activities
Facing down at night will be the most challenging practice you will have to face. But with a little practice, some patience, and some discipline, you will be able to face down effectively. With the use of only one eye, you may experience change in brightness. Having a flashlight handy can help you with some “extra” lighting. Your ability to remain face down while sleeping or awake for extended times depends on how the rest of your body feels. Make sure you are not cluttered on bunched up sheets or having cold feet; this might annoy and agitate you, causing stress. If you have uncontrollable “leaking” from the tear duct, it is very wise to place tissues near your bed in where it is easily accessible.
If sleeping face down with the equipment prior to the surgery can be done, practice sleeping face down. If you feel agitated and uncomfortable, use extra pillows to your sides to help you lay still. An alternative to keeping your face down is to tape a tennis ball to the upper back; if you roll over onto it, you’ll know it.
Pastime Activities
Keeping your head down for seven or more days can get boring. It is helpful if you plan ahead. It is useful to move around. Short walks or light exercise is encouraged. Reading results in a rapid eye movements and is discouraged. We have put together a list that we believe is the best things to do as a pastime activity:
- Listening to music, radio, tapes, CDs, etc.
- Books on tape/CD
- Relaxation tapes/CDs
- Playing with hand squeeze toys
- Playing board games with a partner
- Talking on the phone with speaker capabilities
- Reading/Writing (With a doctor’s permission.)
- Watching TV/Videos/DVDs (With a doctor’s permission.)
(NOTE: Please consult with your doctor about any activities you wish to perform written in this page.)
Reasons and Risks of Vitreoretinal Surgery
The most common condition treated with vitreoretinal surgery is a macular hole with retinal detachment as the second most common condition. Other conditions include macular puckers, macular edema, vitreous hemorrhage and uveitis.
The most common risks associated with vitrectomy are cataracts, retinal detachment, high intraocular pressure, bleeding in the eye and infection.